General Practice 2 Handbook 2023/24
| Site: | QMplus - The Online Learning Environment of Queen Mary University of London |
| Module: | CBME Tutor Site |
| Book: | General Practice 2 Handbook 2023/24 |
| Printed by: | Guest user |
| Date: | Sunday, 1 March 2026, 2:54 PM |
Description
General Practice 2 Handbook
1. Course Administration and Clinical Leads
Contact details for Unit Convenors
Dr Leila Saeed
Maria
Hayfron-Benjamin
m.j.hayfron-benjamin@qmul.ac.uk
Contact details for Unit Administrators
Unit Administrator
Ms Frankie Langridge
f.langridge@qmul.ac.uk
2. GP2 at a glance
Overview of GP2
GP2 is a campus and online-based placement for all Year 2 students at Barts and The London School of Medicine and Dentistry.
This year, the emphasis will be on the fundamentals of general practice (generalism) which will help you understand the principles of general practice as you progress through medical school and afterwards.
GP2 will introduce you to the broader context and key components of General Practice as a speciality and give you an understanding of the professional knowledge.
Mapping of themes
The themes of GP2 and learning outcomes are mapped to:
GMC outcomes for graduates: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates/outcomes-for-graduates
Teaching GP from RCGP: https://www.rcgp.org.uk/getmedia/bd108a4b-50ce-42f0-9de4-c3083a2c8586/teaching-general-practice.pdf
GMC Capabilities Framework: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/generic-professional-capabilities-framework
GMC MLA: https://www.gmc-uk.org/education/medical-licensing-assessment/uk-medical-schools-guide-to-the-mla/mla-content-map
Structure
The 6 themes
There will be 6 themes covered (which is explained in more detail in later chapters).
- Holistic care (biopsychosocial model)
- Long term condition
- Multi morbidity and complexity
- The social determinants of health
- Preventing disease and promoting health
- Medical Ethics
Team based learning (TBL): campus teaching
Team-Based Learning (TBL) is an instructional strategy designed to enhance collaborative learning and critical thinking skills among students in the medical field. It's particularly valuable in the second year of medical school when students are building on foundational knowledge and preparing for clinical rotations.
There is further information in 'TBL section'
Role play: online teaching
You will be split up into groups of 12-15 with a GP tutor on line using Teams. In these sessions, there will be an opportunity to watch real consultations (using Virtual Primary Care), discussions with the GP tutors and practise role plays with actor facilitators.
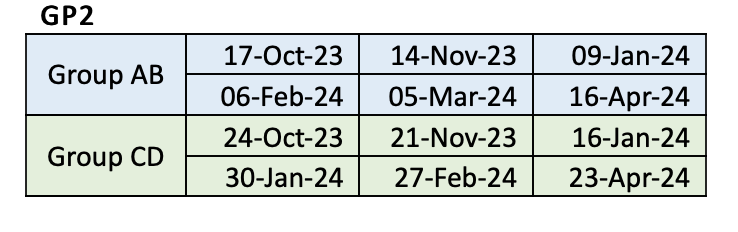
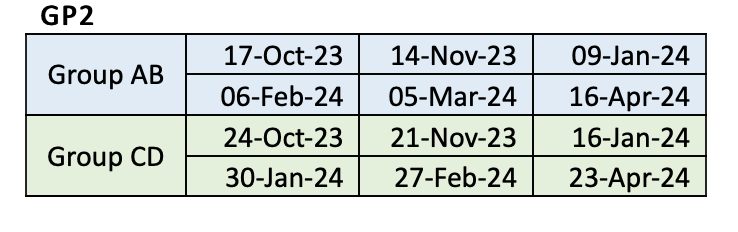
The Dates
3. GP2 aims and objectives
Module Aims:
1. Introduction to General Practice Principles:
- Understand the foundational concepts and principles that guide General Practice as a primary healthcare discipline.
- Explore the role of General Practitioners (GPs) in delivering comprehensive and patient-centered care.
2. Developing knowledge in key themes in GP
- Gain a deeper insight into important elements of GP including: holistic care, long term conditions, multi morbidity, Social determinants of health, promoting health and preventing disease and medical ethics.
3. Clinical Role Play Skills:
- Develop practical skills through role plays that simulate real-life patient interactions.
- Practice effective communication, discussion and debate with fellow colleagues.
4. Patient-Centered Communication:
- Enhance patient communication skills through role plays, focusing on empathy, active listening, and clear information sharing.
- Learn to build rapport and establish a trusting relationship with simulated actors.
5. Professional Development and Reflective Practice:
- Engage in reflective writing to develop skills such as: reflection and an understanding of the importance of continuous learning and growth as a future doctor.
6. Integration of Theory and Practical Experience:
- Apply theoretical knowledge gained from pre-reading material, role plays and Team Based Learning, fostering a deeper understanding of General Practice principles.
4. GP2 TIMETABLE
Dates in more detail:
Day | 1 | 2 | 3 | 4 | 5 | 6 |
Group A | 17/10/2023 AM- TBL PM- role plays
| 14/11/2023 AM- role plays PM- TBL
| 09/01/2024 AM- TBL PM- role plays
| 06/02/2024 AM- role plays PM- TBL
| 05/03/2024 AM- TBL PM- role plays
| 16/04/2024 AM- role plays PM- TBL
|
Group B | 17/10/2023 AM- role plays PM-TBL
| 14/11/2023 AM- TBL PM- role plays | 09/01/2024 AM- role plays PM- TBL
| 06/02/2024 AM- TBL PM- role plays | 05/03/2024 AM- role plays PM- TBL
| 16/04/2024 AM- TBL PM- role plays |
Group C | 24/10/2023 AM- TBL PM- role plays
| 21/11/2023 AM- role plays PM- TBL
| 16/01/2024 AM- TBL PM- role plays
| 30/01/2024 AM- role plays PM- TBL
| 27/02/2024 AM- TBL PM- role plays
| 23/04/2024 AM- role plays PM- TBL
|
Group D | 24/10/2023 AM- role plays PM- TBL
| 21/11/2023 AM- TBL PM- role plays
| 16/01 AM- role plays PM- TBL /2024 | 30/01/2024 AM- TBL PM- role plays
| 2 AM- role plays PM- TBL 7/02/2024 | 23/04/2024 AM- TBL PM- role plays
|
5. ASSESSMENT SUMMARY & SUBMISSIONS
| Submission deadline | Marking deadline | |
|---|---|---|
| Group A | 23rd January 2024 (2 weeks after day 3) |
Marking deadline: 6th Feb 2024 (2 weeks after submission) |
| Group B | 23rd January 2024 (2 weeks after day 3) |
Marking deadline: 6th Feb 2024 (2 weeks after submission) |
| Group C | 30th January 2024 (2 weeks after day 3) |
|
| Group D | 30th January 2024 (2 weeks after day 3) |
13th February 2024 (2 weeks after submission) |
5.1. Reflective essays/creative enquiry
What is reflective writing?
Reflection is a key skill for all healthcare professionals and learning how to develop reflective practice is an essential part of medical education. Creative enquiry has been found to extend reflection and understanding and engage the student voice and perspective [See Appendix 1].
Reflective writing holds significant importance for second-year medical students as it serves as a valuable tool for enhancing their learning, self-awareness, and professional development. This form of writing involves the exploration of personal experiences, thoughts, emotions, and insights related to clinical encounters, patient interactions, and medical practice. Below we have summarised some areas that it incorporates:
Critical Thinking and Decision-Making: Reflective writing encourages students to analyse and evaluate their experiences. This process cultivates critical thinking skills, enabling students to assess the effectiveness of their decisions and discussions. By reflecting on cases and interactions, medical students can identify areas for improvement and make more informed decisions in future situations.
Clinical Skill Development: Through reflection, students can identify gaps in their clinical skills and knowledge. By examining their experiences, they can recognise which skills were effectively applied and which need further development. This self-awareness allows students to focus their learning efforts on specific areas that require improvement, leading to enhanced clinical competence.
Empathy and Patient-Centered Care: Reflective writing encourages students to delve into their emotions and perspectives during patient interactions. This introspection fosters empathy and a deeper understanding of the patient's experience, leading to more patient-centered care. Developing strong interpersonal skills is essential for effective communication and building trust with patients.
Ethical and Moral Development: Medical practice often involves complex ethical dilemmas. Reflective writing provides a platform for students to explore and dissect these ethical challenges, helping them develop a strong moral compass. Engaging in thoughtful reflection can aid in making ethically sound decisions while considering the best interests of the patient.
Self-Assessment and Self-Regulation: Writing reflections allows students to assess their progress and growth over time. They can track their learning journey, identify areas of strength, and set goals for improvement. Regular reflection promotes self-regulation, motivating students to take proactive steps to enhance their knowledge and skills.
Professional Identity: Medical education is not only about acquiring medical knowledge but also about developing a professional identity. Reflective writing enables students to explore their evolving roles as medical practitioners, helping them understand the responsibilities, values, and expectations associated with the profession.
Communication Skills: Effective communication is integral to medical practice. Reflective writing hones students' ability to articulate their thoughts and experiences clearly and concisely. This skill is transferable to patient communication, interprofessional collaboration, and academic discussions.
Resilience and Coping Strategies: Medical training can be emotionally demanding. Reflective writing provides an outlet for processing challenging experiences, managing stress, and building resilience. By acknowledging and addressing emotions through writing, students can develop healthy coping mechanisms and maintain their well-being.
Lifelong Learning: Reflective writing cultivates a habit of lifelong learning. As medical knowledge and practices evolve, physicians must adapt and update their skills. The practice of reflection fosters a mindset of continuous improvement and learning throughout a medical career.
Incorporating reflective writing into your learning as a second year medical student can significantly contribute to your holistic development as future healthcare professionals. By engaging in this introspective process, students not only enhance their clinical competencies but also develop the emotional intelligence and professionalism necessary for a successful and fulfilling medical career.
GP2 Reflective Statement on Teamwork
Introduction:
So far in your GP2 block, you have worked in a team both online [analysing consultations and providing feedback to each other] and in person during TBL [Team based learning]. These team working skills are essential for when you are a junior doctor working on the wards or GP practice, both directly and indirectly affecting patients. These benefits include (however not exhaustive):
· To allow effective and safe management of patients: working together with colleagues and patients for the best patient care i.e. Calling the cardiologist for advice regarding a patient's ECG.
· Conflict resolution: having the skills to work with others to resolve conflict in an effective manner, i.e. You are the GP in an MDT meeting and one of the allied health professionals disagrees with your plan.
· To reduce medical errors: working together to ask questions and clarify i.e. You have been asked to prescribe a medication you are not familiar with, leading to asking the pharmacist for advice.
· Better communication in emergencies, i.e. you are a medical student taking part in a cardiac arrest and have been asked to perform CPR. This involves following instructions from the ‘cardiac arrest team’.
· Better communication amongst team members means reduced stress and improved job satisfaction.
The GMC highlights the importance of communication partnership and teamwork in its Good Medical Practice document. Alongside this, Royal College of Physicians also highlight the importance of teamwork, in the follow document: Improving teams in healthcare.
Purpose of the task:
· This is an opportunity for you to reflect on your team working skills during TBL, understand your role in a team and identify areas to improve on.
The task:
Options:
1. 250–500-word reflective statement on how your TBL/online team worked together to complete a task during GP2 or
2. Creative enquiry – produce a creative piece (poem, drawing, painting) + 250-word piece on how your TBL/online team worked together to complete a task during GP2.
Leniency is +/- 10% of the word count.
Consider:
1. What: What have you learnt about your teamwork skills? Consider how did your team deal with communication, decision-making, and any challenges?
2. Why: Why are team working skills important for your role in the medical profession?
Submission details:
Please submit your pieces to QM Plus (under the General Practice 2 drop down) before the deadline for your group as below. If you have any issues with uploading, please contact Francesca Langridge f.langridge@qmul.ac.uk.
Late submissions will incur penalties
Non submission / inadequate remediation task work may mean the student will forfeit the first sit of the Year 2 exams and will sit in August as a second sit
Deadline:
Group CD: 20th Feb (3 weeks after day 4)
Group AB: 27th Feb (3 weeks after day 4)
The reflective piece will be assessed and graded by one of the GP2 central facilitators.
GP tutors will be asked to submit these marks to the QMUL CBME team and provide both the marks and feedback, written and/or verbal, directly to the students as well.
Mark scheme :
Guidance for grading the reflective pieces
| Merit | Pass | Fail |
Impact | The work moves/engages you. It stays with you/ opens new doors & new perspectives
| There were some interesting insights and perspectives that made you think but could have been explored further. | Themes/ideas addressed superficially. |
Reflection
| Insightful reflection - focussed on ‘key issues/ideas,’ explored from different perspectives, context and emotions are considered.
| Mix of descriptive account with some reflection e.g., the student considers their emotions, looks at the perspective of others, or identifies ‘key issues/ideas,’ but this could be expanded.
| Descriptive account – narrative account of what happened, with little or no reflection.
|
Aesthetics (If creative enquiry piece included) | Excellent use of chosen medium powerfully conveying the content, assisting the audience in engaging with the message. | Some originality. Reasonable effort and use of chosen medium. | Little original thought, little effort, not effective use of medium chosen, not conveying the content well. |
Feedback to students:
It is paramount to students learning that they received feedback, whether this is verbally or written.
Feedback could include:
Points of excellence
Points for improvement - could include questions/prompts to encourage continued reflection
General comments
Consent: Students are asked to confirm whether they give consent for their reflective pieces to be shared, to either include their details or anonymously, for a QMUL creative enquiry website that is being designed to showcase creative enquiry work by QMUL students from all year groups.
See Appendix 3 for further information and links.
5.2. Absences
The medical school are aware that students and GP tutors can be become unwell.The process for students to notify absence is as follows:
1) Fill out a self certifying illness form
2) Notify your GP tutor/TBL tutor
Tutors: If you are not able to do a session for the students, please arrange cover as soon as possible. If this is not possible, please let the student know (this may be via messaging or email) as soon as possible.
5.3. Professionalism assessment
At the end of the GP2 block, all central tutors (from the role plays) will be asked to complete a 'professionalism' form which captures any concerns. Professionalism is a very broad topic, but the general themes that the central tutors will be asked to comment on include:1) Interaction- Did the student interact with the other students? Did they provide feedback to their colleagues? Did they interact with the tutor?
2) Punctual - Were they late on numerous occasions without a valid reason? Did they notify you of their absence/lateness?
3) Camera use - Did they keep their cameras on appropriately? If there was a camera issue, did they provide a valid reason.
4) Attitude- showing respect to fellow colleagues and tutor, and actor facilitator.
Further information can be found in appendix: Professionalism Appendix 2
5.4. Feedback
Engaging with the feedback process is a key part of students’ learning and professional development. This involves learning about both the giving and receiving of constructive feedback and understanding how these feedback processes can support their own, peers and their tutors’, professional development as well as guiding the ongoing development of the placement.
Students and GP tutors/facilitators will be asked to provide feedback about their TBL and central teaching experience via online forms.
Feedback based on the online sessions:
- Students will be asked to submit their feedback about their online experience at the end of the placement. This consists of both individual and group feedback. They will be sent links to these online feedback forms and instructions on how to complete these prior to the final placement days.
- Students are encouraged to approach their GP tutor/facilitator and/or the unit convenors if they have any queries or concerns during their GP2 days.
- Tutors/facilitators will be asked to submit their feedback about their teaching experience at the end of the placement. They will be sent links to these online feedback forms and instructions on how to complete these.
Tutor/facilitator feedback based on reflective essay/creative enquiry
- Tutor/facilitators will be sent online forms for the student assessments as outlined in the assessment information.
Tutor/facilitator feedback based on student consultation performance
- Tutors are also required to provide formative feedback to each student to support the develop of their reflective practice and overall professional development. This also serves to model the constructive giving and receiving of feedback to their students. This formative feedback can be delivered verbally and/or in a written format.
- The use of informal feedback, to review learning experiences and ensure students’ learning needs and the placements learning outcomes are being met, during the placement is encouraged and can be collected as the placement progresses. For example, using Mentimeter to set up anonymous polls or Q&As at the end of each placement day or using post-it notes on Jamboard (or a real whiteboard if onsite).
6. GP2 DAYS IN MORE DETAIL
Below are the 6 themes of GP2, which coincides with each of the GP2 days. These themes are taken from the RCGP/SAPC document 'Learning General Practice': a digital textbook for clinical students.
The themes are also mapped across 'GMC Outcomes for graduates', MLA and Generic professional capabilities framework (GMC). These recommendations are further looked at in each TBL theme section.
- Holistic care (biopsychosocial model)
- Long term conditions
- Multi morbidity and complexity
- The social determinants of health
- Preventing disease and promoting health
- Medical Ethics
Note each theme has a hyperlink to QM Plus with all the pre-reading information, videos and structure of the day.
Also note that this handbook is updated live before each session, hence not all individual day information will be available until 1 week before.
6.1. Preventing disease and promoting health
Summary of session:
This week’s topic for Team Based Learning will be on preventing disease and promoting health. This is a key element of medicine and in particular general practice and primary care, where 90% of clinical contacts take place. Medicine is rapidly shifting towards a preventative approach at local, national and global level, and our learning should reflect this.
Learning objectives:
By the end of this session, you should be able to:
Understand the benefits of health promotion and disease prevention in the context of the specific patient population
Describe methods by which we can prevent disease and promote health
Describe and explain benefits of specific public health interventions such as targeting smoking cessation, reducing obesity and the harm caused by alcohol abuse, dietary interventions and increased physical activity
Apply public health principles to a local population and their specific needs
Have gained greater awareness of the global and multicultural aspects of delivering evidence-based, sustainable healthcare.
Link for the QM Plus TBL session
**Will be added in run up to session**
6.2. The social determinants of health
Start to evaluate the environmental, social, behavioural and cultural factors which influence health and disease in different populations
Start to assess, by taking a history, the environmental, social, psychological, behavioural and cultural factors influencing a patient’s presentation, and identify options to address these, including advocacy for those who are disempowered
Start to evaluate the determinants of health and disease and variations in healthcare delivery and medical practice from a global perspective and explain the impact that global changes may have on local health and wellbeing.
Link for the QM Plus TBL session
**Will be added in run up to session**
6.3. Holistic medicine/biopsychosocial
Summary of session:
Holistic care is about seeing the patient as a ‘whole’. This is a concept practiced by GPs daily, as we are normally at the centre of the patient's care. Holistic care involves looking at the patient from the point of view of physical, social and mental aspects of health (known as biopsychosocial model). In most (but not all) cases, these different areas may overlap and interact, and so rather than looking at individual areas, it is paramount consider all areas.Short line about the different section.
Learning Objectives
1. Identify the core principles and components of holistic care in the medical field.
2. Analyse the importance of incorporating holistic care in the overall management and treatment of patients.
3. Explore the potential benefits and limitations of using holistic care approaches in medical practice.
4. Apply a holistic care framework to assess and address the physical, emotional, social, and spiritual needs of patients.
5. Evaluate the role of effective communication and empathy in establishing trust and rapport with patients in a holistic care context.
6. Collaborate with team members to develop comprehensive and patient-centered treatment plans that integrate holistic care principles.
7. Examine the impact of cultural, ethnic, and socioeconomic factors on the provision of holistic care and health outcomes.
8. Discuss ethical considerations and potential challenges associated with incorporating holistic care into standard medical practice.
9. Engage in critical thinking and problem-solving exercises to analyse case studies or scenarios that require the application of holistic care principles.
Link for the QM Plus TBL session
**Will be added in run up to session**
6.4. Multi morbidity and complexity
Summary of session:
Multi morbidity is the norm for most GP consultations now, as we have a higher proportion of elderly patients with multiple conditions living longer. These numbers are increasing and is largely connected to health and economic deprivation.
Learning Objectives
1. Understand the concept of multi-morbidity:
2. Recognise medical complexity:
- Define medical complexity and its various dimensions (e.g., medical, social, psychological).
- Identify factors that contribute to medical complexity, such as age, socioeconomic status, and healthcare access.
3. Comprehend the challenges in managing multi-morbid patients:
- Identify the potential complications and interactions between co-existing medical conditions.
- Describe the impact of polypharmacy in multi-morbidity management.
- Understand the role of healthcare system and provider factors in managing medical complexity.
4. Strengthen communication and teamwork skills:
- Understand the importance of interdisciplinary teamwork in managing medical complexity.
5. Engage in self-directed learning and continuous improvement:
Link for the QM Plus TBL session
**Will be added in run up to session**
6.5. Long term conditions
Short line about the different section:
Learning objectives:
By the end of this session, you should be able to;
What are we trying to achieve
Students' awareness of LTC
Debate the impact of LTC on patients' life
What are the learning outcomes:
Students to recognise the impact of LTC on patients
To draw upon a real-life scenario
Students to think about different LTC within the community
Students to look at different roles of HCP involved in patients with LTC
Link for the QM Plus TBL session
**Will be added in run up to session**6.6. Medical ethics
Learning Objectives
1. Understanding the Basics of Medical Ethics:
- Define medical ethics and its significance in healthcare.
2. Ethical Principles in Healthcare:
- Describe the four fundamental principles of medical ethics: autonomy, beneficence, non-maleficence, and justice.
- Provide examples of how these principles guide medical decision-making.
3. Informed Consent:
- Define informed consent and its role in medical practice.
- Explain the elements necessary for obtaining valid informed consent.
4. Cultural Competency and Ethical Care:
- Recognise the importance of cultural competence in delivering ethical healthcare.
- Discuss how cultural beliefs and values can impact healthcare decision-making.
5. Case Studies and Group Discussions:
- Provide opportunities for students to analyse ethical cases and engage in group discussions to develop their ethical reasoning skills.6. Communication and Ethical Decision-Making:
- Emphasise the role of effective communication in addressing ethical issues with patients, families, and colleagues.
- Discuss strategies for resolving ethical conflicts in a collaborative manner.
7. Professional Codes of Ethics:
- Familiarise students with professional codes of ethics relevant to medical practice (e.g., GMC Code of Medical Ethics).
- Highlight the importance of adhering to these codes in their future careers.
8. Reflection and Self-Assessment:
- Encourage students to engage in self-reflection on their personal values and how they may impact their ethical decision-making as future healthcare providers.
Link for the QM Plus TBL session
**Will be added in run up to session*
7. Team Based Learning
Team-Based Learning (TBL) is an instructional strategy designed to enhance collaborative learning and critical thinking skills among students in the medical field. It's particularly valuable in the second year of medical school when students are building on foundational knowledge and preparing for clinical rotations.
It was first introduced in the business school environment by Dr Larry Michaelsen.
The concept is based around pedagogy and flipped classroom approach.
.png)
Please refer to the following useful resources:
Mandatory E-Learning module (20 minutes)
Professor Graham Easton has put this extremely informative E Learning module together that outlines TBL.
https://qmplus.qmul.ac.uk/course/view.php?id=21922
Short video by LAMS
https://docs.lamsfoundation.org/tbl/tbl-with-lams
Student orientation:
Thursday 12th October 2023 - Bearsted lecture theatre
A+B: 15:00-17:00
C+D 9:00-11:00
7.1. What is TBL?
Here's a breakdown of TBL:
1. Formation of Teams: Students are divided into small, diverse teams. This diversity encourages the exchange of different perspectives and expertise. You will be notified of your groups by Francesca Langbridge before your sessions.
2. Pre-Class Preparation: Before each TBL session, students are assigned readings or materials related to the topic. This pre-class work helps students familiarise themselves with the content. The prep time can vary from 1-2 hours made up of a combination of written information, videos and links to websites.
3. Readiness Assurance: In the initial phase of the TBL session, students take an individual readiness assessment test (IRAT) to gauge their understanding of the pre-class material. This test is followed by a team readiness assessment test (TRAT), where teams work collaboratively to answer the same questions.
4. Immediate Feedback: The immediate feedback process allows students to discuss and debate their answers with their teams and receive instant clarification from the instructor. This fosters peer teaching and reinforces understanding.
5. Application Activities: After the readiness assurance phase, students engage in application activities. These can include case-based discussions, problem-solving exercises, or simulations related to the medical topic. Teams work together to apply their knowledge to real-world scenarios.
6. Instructor Facilitation: The instructor's role in TBL is to guide discussions, provide clarifications, and ensure that the learning objectives are met. They act as a facilitator rather than a traditional lecturer.
7. Reflection and Discussion: TBL encourages students to reflect on their learning process and engage in discussions about the application of knowledge. This promotes critical thinking and deeper understanding.
7.2. Why are we using TBL?
TBL has its many advantages including promoting:
1) Active learning
2) Teamwork
3) communication skills
4) Critical thinking.
It prepares medical students for clinical scenarios where collaboration and problem-solving are essential.
However we do recognise that it does come with its challenges, which may be a new way of learning and adjustments to the traditional lecture-based approach or practice based learning. We do hope it is enjoyable and a great learning experience for all.
7.3. TBL resources
TBL resources:
Mandatory E-Learning module (20 minutes)
Professor Graham Easton has put this extremely informative E Learning module together that outlines TBL.
https://qmplus.qmul.ac.uk/course/view.php?id=21922
Short video by LAMS
8. Online: Role Plays and VPC
We have already discussed TBL, but now let's think about the other half of the day (which may be AM or PM). This part of the day, referred to 'central or online' is made up of online activities facilitated by a central tutor.
The sessions are 3 hours long and consist of 1-2 recorded GP consults (virtual primary care) followed by 4 role plays.
Role plays with actor facilitators are a great way to practice your communication skills and receive/give feedback from/to colleagues.
Topics:
The roles may be related to the TBL topic but not exclusively. This is to avoid being reliant on TBL material to do the role plays i.e. you may have role plays in morning but TBL in afternoon. The most important aspect of this, is that you get to watch and practice consulting with actors, and gain the confidence to speak to patients.
The TBL topics will naturally reinforce your knowledge and work alongside the central topics.
Resources:
The resources for the role plays will be added a week before each session on Teams. You will have been allocated a Teams group i.e. Orange group A or Red group D. We aim to keep the the groups the same for the whole GP2 block (but if for unforeseen circumstances i.e. Tutor absence, certain groups may have to join with other groups).
Virtual Primary Care (VPC)
https://vpc.medicalschoolscouncil.org.uk/
All students will be given access to VPC which is required for the central online sessions. If you have any issues with access - please email Frankie on:
f.langridge@qmul.ac.ukSee appendix 4 - Role Plays for feedback forms.
9. Appendices
Further information
9.1. Student support: IHSE Student Support (formerly known as SAPS)
IHSE Student Support:
If you are struggling with the course or have any concerns, please speak to your central tutor or to the module leads (Dr Leila Saeed). If you feel that your query requires further input, student support information can be found below:
9.2. Professionalism
The term professionalism can be difficult to define but outlines particular principles all medical students and health care professionals should abide by in order to safely practice medicine.
Professionalism may also be connected to be 'conscientiousness' - which is based around the idea of being persistent, organised and motivated. .
Professional looks at traits that are linked with the following:
1) Ethical behaviour - Although you may not be interacting with 'real patients' who we present ourselves to others i.e. our colleagues, GP tutor and actor, should be consistent with the following principles: honesty. integrity and respect.
2) Professional appearance - dress code should be appropriate. Further information can be found on Queen Marys website.
3) Time management - ensuring you are punctual to respect yours and others time.
4) Teamwork - working effectively as a team.
5) Accountability - Students should take responsibility of their own learning and learn from mistakes.
6) Self care - Students should take care of their own health and recognise when they are not well enough to attend sessions. This includes physical and emotional burnout and illness. All students should be registered with a GP.
7) Reflection and improvement
It is advised that all students read the Good medical practice - GMC, which outlines the standards expected of medical students.
9.3. Learning through reflection and creative enquiry
Reflection is a key skill for all healthcare professionals and learning how to develop reflective practice is an essential part of medical education. The GMC (General Medical Council), in collaboration with the Academy of Medical Royal Colleges, the UK Conference of Postgraduate Medical Deans (COPMeD), and the Medical Schools Council (MSC), recently published a guide for medical students on how to reflect as part of their practice.
The key idea of reflective work is to promote self-awareness. It enables students to explore their understanding of themselves as medical professionals and how they relate to patients. It also provides a space where students can consider and challenge their own attitudes and perceptions, including highlighting learning points for themselves and others.
There are many formats that can be used for reflection, including verbal, written and art. Creative enquiry is an educational approach that invites learners to engage with their lived experience through the arts. Using multiple languages of expression, arts-based and prose reflective writing, has been found to extend reflection and understanding and engage the student voice and perspective.
Resources for reflections:
Here are some resources for reflection that you may find helpful:
From QM Plus:
The websites, Human Flourishing and Out of Our Heads, have more information about creative enquiry and lots of examples.
9.4. Role Play feedback
Student Name: ........................................ Date: ..................
Skill Examples Feedback
Introduction & Orientation | Full name and role. Name preference. Checks patient’s comfort. Explains purpose of interview. Confidentiality including notetaking. Seeks consent to continue. Welcoming manner. | |
Patient backstory | Provides the ‘Golden Minute’: encouraging the patient to tell their story. Elicits a timeline of events. Shows respectful curiosity about the patient. | |
Patient Perspective | The patient’s ideas, concerns and expectations. ‘What matters to the patient?’ | |
Content - biomedical perspective | Adequately explores information needed for diagnosis or management. This includes both bio/medical and psycho/social content. ‘What is the matter with the patient?’ | |
Engagement | Shows interest, respect and concern. Responding to patient’s answers. Picks up on patient’s cues. Asks appropriate questions (open & closed) | |
Empathic Responses | Reflecting back and acknowledging patients’ feelings and concerns as expressed in the interview. | |
Appropriate Reassurance | Handles uncertainty appropriately. Refrains from false or premature reassurance. Offers appropriate reassurance or help. | |
Organisation | Systematic and logical flow, signposting and summarising. Guiding the patient through the consultation. | |
Closure | Summarises main points to ensure everything is covered. Explains next steps (if applicable). Thanks patient. |
Student Name: ........................................ Date: ..................